
February 2024
The Top 10 Developments in Drug Insurance of 2023
A look back at the highlights of 2023 in this ninth edition of our top drug insurance developments of the past year.
EVOLUTION OF PUBLIC PLANS
1. Switch to biosimilars gaining popularity
2. Free contraceptives: British Columbia paves the way
3. Opioid crisis: the death toll continues to rise
4. National pharmacare: no agreements in 2023
EQUITY, DIVERSITY AND INCLUSION
5. Family planning: insurers expand their offerings
6. Ozempic: the drug on everyone’s lips!
7. Weight management medications
OTHER HIGHLIGHTS
8. Dispensation of specialty drugs – A tale of two worlds in Canada
9. Trikafta: a flagship product
10. ADHD drugs: significant increase in claimants
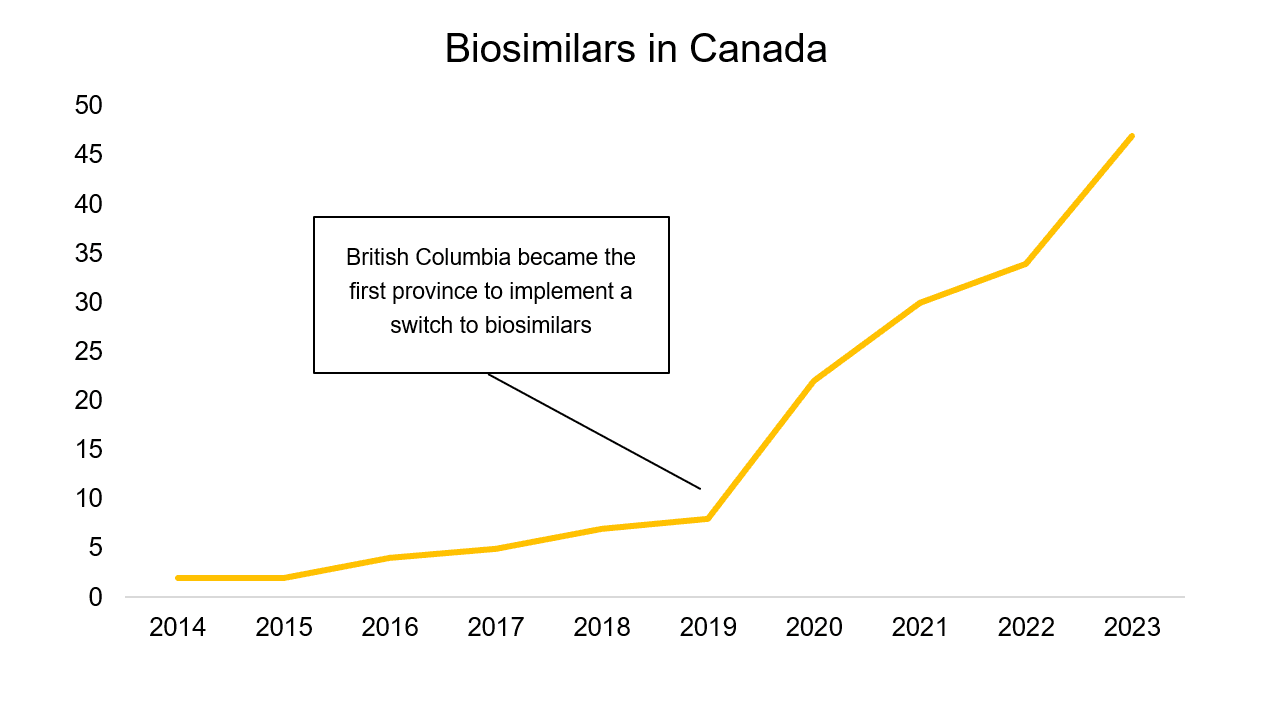
In 2023, Canadian provinces continued their shift towards the use of biosimilar medications. Nova Scotia, Newfoundland and Labrador, Ontario, Yukon, and Saskatchewan officially joined the national movement this year.
Prince Edward Island will join the other Canadian provinces and territories when the transition period ends in June 2024. The governments of Manitoba and Nunavut, on the other hand, have not yet announced their intentions.
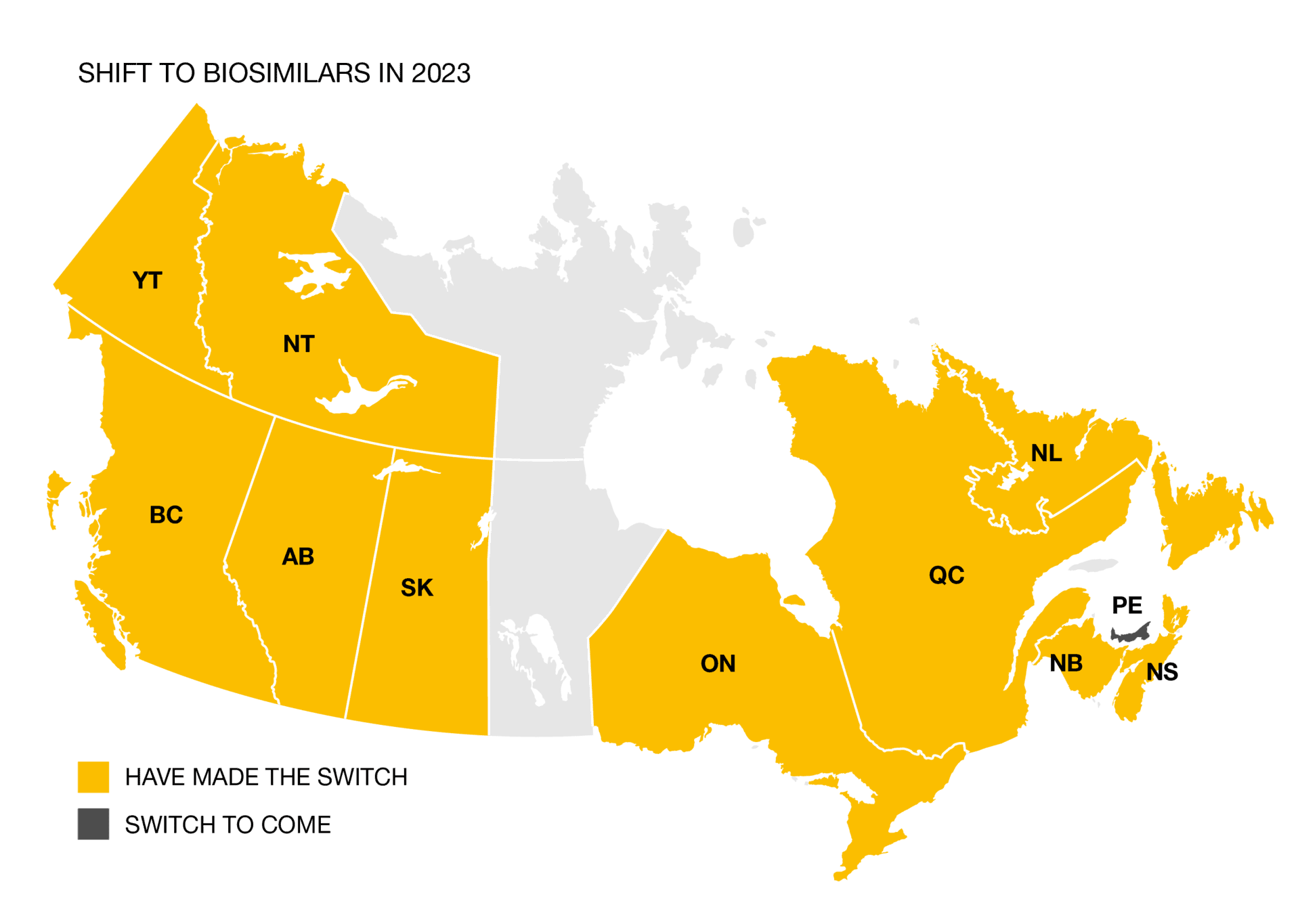
Since the provinces began shifting towards the use of biosimilars, the supply has greatly expanded in Canada. More than 40 different biosimilar drugs are now approved by Health Canada.
On April 1, 2023, British Columbia became the first Canadian province to offer prescription contraceptives free of charge. These products represent approximately 2% of the total drug expenditure for private insurance plans in British Columbia. This will therefore lower the costs of British Columbia’s private insurance plans.
This measure covers not only contraceptive pills, but also most injections, copper and hormonal intrauterine devices, subcutaneous implants, as well as the Plan B pill (commonly known as the morning-after pill).
Also, since June 1, 2023, pharmacists in British Columbia can prescribe certain medications, including contraceptives.
Canadian companies could see this as an opportunity to cover more contraceptive devices, as British Columbia does, in order to ensure better equity among their staff.
A worsening scourge
The number of deaths related to opioid overdoses continues to rise across Canada, with Ontario, British Columbia, Alberta, and Quebec being the worst affected (in that order).
Actions taken by insurance companies
In constant evolution, proactive opioid management programs offered by insurers generally involve implementing two measures: restricting the supply to seven days to start treatment and encouraging insured individuals to start with a short-acting opioid (except in cases of cancer and when the medical profession prescribes long-acting opioids as first-line treatment).
Measures taken by British Columbia
British Columbia, the province with the second-highest overdose death rate, has already filed a class action lawsuit against several pharmaceutical companies that made false statements about the risk of addiction and the adverse effects of opioids. The Quebec government is considering joining this class action lawsuit. On June 6, 2023, British Columbia became the first province to implement a universal program covering opioid withdrawal treatments for residents with active medical coverage.
As part of the supply and confidence agreement reached between the Liberals and the New Democratic Party (NDP), a first bill regarding the national pharmacare program was supposed to be adopted in 2023. A first draft of the bill, rejected by the NDP last fall, suggests that there will be more discussions on this subject in 2024.
A first step toward national pharmacare was made in 2022 with the signing of the funding agreement between the federal government and Prince Edward Island. This $35 million investment over four years has already allowed the province to make certain medications more accessible to its population. Several changes to the provincial plan also came into effect on July 1, 2023, including reducing the maximum out-of-pocket expenses for residents.
For more information on Normandin Beaudry’s position on national pharmacare, consult our white paper.
Provincial coverage for fertility treatments in Canada is quite limited, only covering a portion of the costs for many families for medications or other expenses (e.g., in vitro fertilization). Furthermore, this coverage can vary greatly from one province to another.
In 2023, insurers have significantly expanded their offerings of family planning programs in order to provide employers with the opportunity to add these products to their group benefits coverage, resulting in more comprehensive and equitable coverage for their employees across Canada. Most coverage options reimburse medications and other expenses related to fertility treatments.
Insurers have deployed various cost management measures to ensure that Ozempic, approved by Health Canada to treat type 2 diabetes, is prescribed for that purpose only, and not for weight loss despite its proven efficacy.
Significant cost increase in 2022 and 2023
This medication represents a significant portion of drug insurance plan expenses. In the market, we’ve observed that the expenditure for this medication has doubled every year for several years. Ozempic has become a top-selling drug in Canada over the past year.
Insurers’ cost control measures
Even though some insurers already had sound cost management measures for Ozempic (prior authorization and step therapy), many of them implemented some measures in 2023 for the first time to ensure that this medication is reimbursed only for type 2 diabetes and not for weight loss.
Please note that new drug Mounjaro, approved by Health Canada in the fall of 2023 as a treatment for type 2 diabetes, will be subject to the same cost management measures as Ozempic.
The next step for plan sponsors is to take position on weight management drug coverage, given that many plans do not provide coverage for these medications.
Wegovy (a medication made from the same molecule as Ozempic, but with a higher dosage) has been approved by Health Canada since late 2021 for weight loss purposes. However, this promising drug has yet to enter the Canadian market due to supply shortages. While other medications are available on the market, Wegovy remains highly anticipated in 2024.
Currently, Canadian public health plans do not cover weight management medications. Historically, private plans have followed the example of public plans and, even today, the vast majority of plans do not cover these medications. However, a growing number of plans have been covering these medications in recent years, for various reasons.
Although providing coverage for these medications leads to a direct increase in the costs of a plan, it could also lead to savings elsewhere, particularly by reducing hospitalizations, absenteeism, and costs related to heart disease treatment.
In the interest of fairness, organizations want to ensure that they provide medication coverage for all health issues, without discrimination. In 2023, some insurers have indeed decided to cover weight loss medications in all their contracts, offering an option for plan sponsors to remove them.
Specialty medications can be a significant financial burden for individuals with complex illnesses, which is why Patient Support Programs (PSPs) have emerged in recent years. These programs, funded by pharmaceutical companies, provide financial support combined with comprehensive care at every stage of therapy.
In recent years, some PSPs established partnerships with specialty pharmacies. In Quebec, the code of ethics of the Ordre des pharmaciens du Québec prohibits obtaining clients through an intermediary, with some specialized pharmacies being sanctioned in 2023 and in recent years. Outside Quebec, there are no laws ruling out these agreements.
In order to save money and provide support to patients, several insurers partner with specialty pharmacies to dispense specialty medications. However, this offer is not available in Quebec, which creates inequities for plan sponsors across Canada.
| Specialty pharmacies dispense specialized medications and advise patients on how to use them. |
Trifakta has been making headlines in recent years thanks to its effective treatment of cystic fibrosis. We are seeing a significant increase in the expenditure for this medication in group benefits plans, and it is now among the top 10 selling medications in Canada.
The medication, approved by Health Canada in June 2021 for individuals aged 12 and older, is only reimbursed for patients carrying at least one copy of the delta F508 mutation of the CFTR gene, which represents 90% of people with cystic fibrosis in Canada.¹ Since April 2022, the medication has been reimbursed for children aged 6 to 11, and in October 2023, Health Canada approved Trikafta for children aged 2 to 5. The expansion of coverage will lead to an increase in spending for this expensive medication in private plans in the coming years.
Historically, medications for attention deficit hyperactivity disorder (ADHD) were primarily used by children.
In recent years, the number of adults consuming ADHD medications has skyrocketed. In 2023, the use of medications to treat ADHD was nearly equal among children and adults in the Canadian market.
Several reasons can explain this increase, including greater social acceptability, better diagnostic tools, or the fact that consumption continues into adulthood.
The increase in the number of people who have submitted claims in recent years has put upward pressure on the cost of group benefits plans. The upcoming arrival of a generic version of Vyvanse, one of the most widely used medications for ADHD, could help control costs in the future.
Would you like more information? Contact your Normandin Beaudry expert or email us.
¹ CYSTIC FIBROSIS CANADA. TRIKAFTA, [Online]. [https://www.cysticfibrosis.ca/our-programs/advocacy/access-to-medicines/trikafta].
